Dragana Marković1,3,*, Eleonora Čapelja2
1Department of Chemistry, Biochemistry and Environmental Protection, Faculty of Sciences, University of Novi Sad, Trg Dositeja Obradovića 2, 21000 Novi Sad, Serbia; markovic.dragana215@gmail.com
2Department of Biology and Ecology, Faculty of Sciences, University of Novi Sad, Trg Dositeja Obradovića 3, 21000 Novi Sad, Serbia; eleonora.capelja@dbe.uns.ac.rs
3Association for the International Development of Academic and Scientific Collaboration
*Correspondence: Dragana Marković, markovic.dragana215@gmail.com
– published as website article, to be included in the Volume 1, Issue 1 of the AIDASCO Reviews –
ABSTRACT: Major depressive disorder (MDD), also known as clinical depression, is a serious mental disorder and ranks first among psychiatric disorders that dominate the global disease burden. Recently, it was found that psilocybin, active compound derived from psychotropic mushrooms, can relieve depression symptoms rapidly and sustained benefits for several months. Beside MDD, psilocybin can alleviate symptoms of anxiety, and post-traumatic stress disorder. In the human body, psilocybin is dephosphorylated to form its active metabolite, psilocin which exhibits its effect through binding to various serotonin receptors. Is is considered relatively safe and can potentially meet the therapeutic needs without addictiveness and overdose risk. Although psilocybin has great potential in treating MDD and other psychological disorders, many studies so far lack homogeneity in their methodology, which limits conclusions. Further studies are needed in more extensive and diverse populations.
Keywords: Psilocybe; Psilocin; Medicinal and hallucinogenic mushrooms; Treatment of depression; Psychiatric disorders
1. Introduction
Major depressive disorder (MDD), also known as clinical depression, is a serious mental disorder that affects approximately 300 million individuals worldwide and ranks first among psychiatric disorders that dominate the global burden of disease [1,2]. Neurotransmitter-related abnormalities, including the neuromodulators serotonin, noradrenaline, and dopamine, characterize MDD. One of the main strategies in the pharmacological treatment of MDD involves the inhibition of the reuptake of monoamines, particularly serotonin and/or noradrenaline [3]. Accordingly, selective serotonin reuptake inhibitors (SSRIs) and monoamine oxidase inhibitors (MAOIs) are first-line pharmacological treatments for depression [4]. However, these antidepressants, like many others, have many side effects, including headaches, gastrointestinal problems, sedation or insomnia, anxiety, memory, cognitive impairment, suicidal ideation, activation and aggravation of psychosis, etc. [5]. Antidepressant medications and cognitive behavioral therapy can be effective for some patients, but around 20% do not respond to any intervention, and many who do respond, eventually relapse [6]. Therapeutic deficiencies with antidepressants invite the need to identify and develop novel rapid-acting antidepressants. Psilocybin is recently shown to relieve depression symptoms rapidly and with sustained benefits for several months [2].
Psilocybin is an indole alkaloid found in more than 200 species of mushrooms with global distribution. Genus Psilocybe is the main source of this compound, but some species from the genera Panaeolina, Pluteus, Panaeolus, Stropharia, Conocybe, and Gym-nopilus also contain psilocybin in lower concentrations [7,8]. Psilocybin, the active ingredient found in hallucinogenic mushrooms, also called “magic mushrooms”, is a powerful psychedelic. It has the ability to change the perception of space and time, causing visual distortions, euphoria, and mystical experiences. In the human body, psilocybin is dephosphorylated to form its active metabolite, psilocin. Psilocybin and psilocin are structurally analogous to the neurotransmitter serotonin. Psilocin reacts agonistically with many serotonin receptors, especially serotonin 5HT-2A receptors. Agonist activity of the 5HT-2A receptor is generally considered a key pharmacological mechanism for inducing hallucinogenic effects, which mediates its anti-depressant and anti-anxiety effects. Contemporary scientific reports have indicated the therapeutic use of psilocybin to treat mental health disorders such as MDD, anxiety, and post-traumatic stress disorder. Psilocybin may potentially meet the therapeutic needs for many indications, including depression, without addictiveness and overdose risk [6,8,9].
2. From ancient magic to modern medicine
Psilocybin as a medical substance has a long history through the traditional consumption of hallucinogenic mushrooms in religious and spiritual ceremonies in ancient world cultures. The use of hallucinogenic mushrooms may have started during periods of extreme food scarcity when hungry hominins were trying to find new food. The repeated use of these mushrooms was probably supported by their low toxicity and psilocybin close resemblance to the neurotransmitter serotonin, which caused positive and euphoric experiences. Mushrooms have been used for healing, anesthesia, and celebrations [10]. Despite thousands of years of use, the earliest written record of the use of these mushrooms is in the Florentine Codex, which mentions sacred mushrooms called teona-nácatl, used in Aztec spiritual works. Robert G. Wasson introduced western science and a broad audience to these mushrooms, after attending a Mazatec ritual, and he shared his experiences in a “Life” article called “Seeking the Magic Mushroom”. Mycologist Roger Heim last systematically ranked them, and samples were sent for analysis to the chemist Albert Hofmann [3,11]. Psilocybin was first isolated and identified from mushrooms (Psilocybe mexicana) by Hofmann in 1957, and in 1958 was produced synthetically for the first time [12].
In the 1960s, psilocybin was widely used in the experimental research of mental disorders and showed a little propensity for habit formation, overdoses, or addictiveness. Scientists realized the potential of psilocybin in neuroscience and psychiatry. Unfortunately, psilocybin containing mushrooms spread amongst the general public and became a popular recreational drug. The non-medical use and connection with the hippie trend caused a political reaction, due to which research with classic psychedelics lost financial support from state institutions and stopped. It was not until the beginning of the twenty-first century that scientific interest in psilocybin returned. This was driven by the fact that conventional medicine was ineffective enough and expressed various side effects. Since then, significant advances have been made in characterizing the chemical properties of psilocybin as well as its therapeutic uses [7,13].
3. Mechanism of action of psilocybin
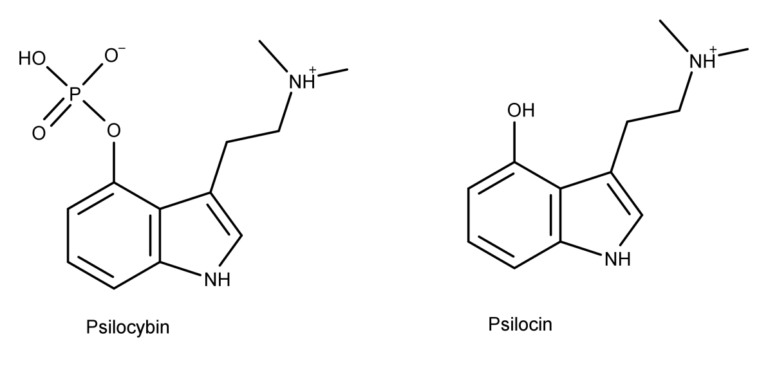
How does psilocybin act on the brain and achieve its effects? Although this process is not fully understood, research shows that psilocybin first changes into its active form – psilocin. When ingested, psilocybin (4-phosphoryloxy-N,N-dimethyltryptamine) is rapidly dephosphorylated to psilocin (4-hydroxy-N,N-dimethyltryptamine) by alkaline phosphatase in the liver and nonspecific esterase in the intestinal mucosa [9,14]. Psilocybin and its metabolite psilocin (Fig. 1) structurally belong to the group of tryptamine/indolamine hallucinogens and are serotonergic psychedelics that produce an atypical state of consciousness characterized by altered perception, cognition, and mood [15].
Like all serotonergic psychedelics, psilocin reacts agonistically with serotonin (5-hydroxytryptamine) type 2A (5HT-2A) receptors to produce hallucinatory effects (Fig. 2). 5-HT serotonin receptors are densely located in areas of the brain responsible for mediating mood and anxiety disorders, such as the prefrontal cortex. Psilocin binds with high affinity to 5HT-2A serotonergic receptor subtype, but studies have confirmed that there is also an affinity for 5HT-1, 5HT-4, 5HT-5, 5HT-6, and 5HT-7 receptors.
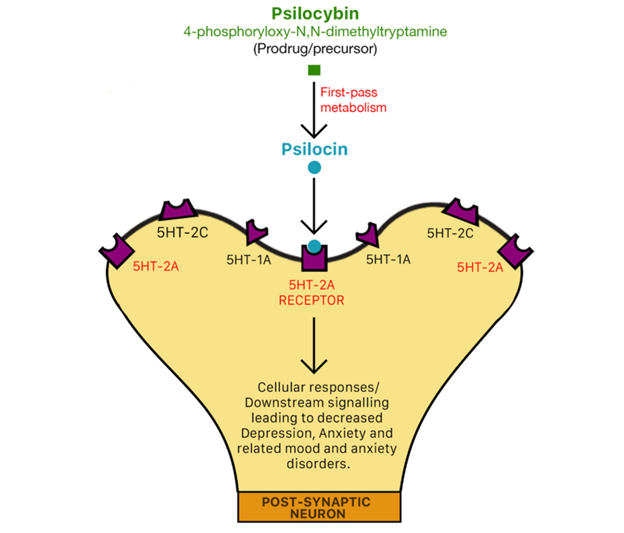
It was determined that overexpression of 5HT-2A receptors in MDD patients positively correlates with both severity and duration of depression, so psilocin ability to lead to desensitization and downregulation of receptor density presents its main antidepressant activity [7,14,15]. In addition, agonism of the 5HT-2A receptor leads to an increase in extracellular glutaminergic concentrations in the prefrontal cortex, which also aids in the antidepressant effects. It is also established that indirect effects on the dopaminergic system contribute to and affect other lower-affinity targets [16,17]. Data presented in the murine study suggest that psilocin has been shown to increase the concentrations of extracellular dopamine. This presents yet another possible mechanism of the antidepressant action of psilocybin: the ability to increase dopamine, a neurotransmitter responsible for regulating emotions and even an individual’s physical well-being [18].
Along with the direct effects on neurochemical systems, psilocybin alters neural circuitry and key brain regions previously implicated in depression, including the default mode network and amygdala. The amygdala plays an essential role in perception and emotion-processing networks. In cases of MDD, an individual typically loses responsiveness to emotional stimuli. This suggests that psilocybin may have significant potential in the treatment of MDD [7].
4. Clinical studies
Many studies suggest that psilocybin-assisted treatment produces substantial anti-depressant effects in patients with MDD. In one study, 12 patients (six men, six women) with moderate to severe treatment resistant MDD received two oral doses of psilocybin (10 mg and 25 mg, 7 days apart). Psilocybin’s acute psychedelic effects typically became detectable 30–60 min after dosing, peaked 2–3 h after dosing, and subsided to negligible levels at least 6 h after dosing. All patients tolerated psilocybin well, and no serious or unexpected adverse events occurred. Depressive symptoms improved even after three months [6].
Other clinical research has shown that one or two doses of psilocybin rapidly alleviate depressive symptoms, with a therapeutic benefit lasting for 12 months [19,20]. One of these researches included 24 patients with moderate to severe MDD who received two doses of psilocybin with supportive psychotherapy. Patients reported mild adverse effects such as transient headaches, anxiety, confusion, and nausea. There were no clinically significant adverse events to be related to psilocybin in the long-term follow-up period, and no participants reported psilocybin use outside of the study. Patients’ ratings of personal meaning and experience after sessions predicted increased well-being at 12 months and did not predict improvement in depression [20].
Despite these promising results obtained in studies with small number of patients, when the number of participants increases, so does the number of reported adverse effects. In a study by Goodwin et al., where three experimental groups were formed (79, 75, and 79 participants received 25 mg, 10 mg, and 1 mg of psilocybin, respectively), it was determined that the group who received 25 mg of psilocybin had significantly better MADRS (Montgomery–Åsberg Depression Rating Scale) total score than within 1 mg dose group. Still, there was no significant difference between the 10 mg and 1 mg dose groups. Adverse effects were reported on day one, day two, and up to week three after taking psilocybin and were present in all three experimental groups, with the 25 mg dose group having the highest percentage of adverse events and severe adverse events reported. Besides headaches, nausea, dizziness, and fatigue, some participants had suicidal ideas or self-injurious behavior [21].
Alongside investigations of using psilocybin for treating MDD, one trial reported the feasibility and safety of administering moderate doses of psilocybin to patients with cancer related depression. In this placebo-controlled crossover trial, 29 patients were randomly assigned and received treatment with single-dose psilocybin (0.3 mg/kg) or niacin, both in conjunction with psychotherapy. Psilocybin produced rapid anxiolytic and anti-depressant effects in patients with cancer related psychological distress [22].
The neural effects of treatment with psilocybin within participants with MDD and healthy controls include a varying degree of changes in neural activation and connectivity in distinct neural regions. For example, in one study, fMRI (functional magnetic resonance imaging) scans revealed that amygdala activity was significantly reduced and was correlated with the positive mood in the 25 healthy volunteers who were given psilocybin [23]. Reduction of amygdala activity following psilocybin administration was also observed in several other studies [24,25]. These findings may be important for MDD patients since amygdala activation increases during depressive episodes [1].
Results of randomized clinical trials demonstrated the efficacy of psilocybin-assisted therapy in producing significant, rapid, and sustained antidepressant effects among patients with MDD. Due to the low physiological toxicity, low abuse/addictive liability, safe psychological responses, and no associated persisting adverse physiological or psychological effects during or after use, psilocybin may provide new and significant opportunities in the conventional treatment of psychiatric disorders, including MDD. However, some limitations must be overcome before they become an established part of psychiatric treatment. These limitations include global history, lingering negative stigmatization of psychedelic drugs, and lack of more extensive, randomized clinical studies to assess safety, pharmacology, and therapeutic dose. Additional limitations to psilocybin pharmaceutical research include a lack of data on psilocybin–drug interactions and combination-medicine studies, a lack of data on the effects of psilocybin on brain activity/dynamics/structure and data on the molecular effects of psilocybin and a lack of data mechanism of action behind persisting positive effects after psilocybin treatment [7,20].
5. Conclusions
Psilocybin has great potential in treating MDD, but many studies so far lack homogeneity in their methodology, which limits conclusions. Further studies are needed in more extensive and diverse populations. Risks associated with psilocybin may be prevented or alleviated by psychologist counseling to induce the right patient mindset and adequate professional clinical psychological support. The future of psilocybin-based pharmaceuticals may involve the general research and development of psilocybin drugs, combination therapy of psilocybin with other drugs, and conventional psychotherapy. Microdosing psilocybin is an area that deserves exploratory and larger-scale clinical study. It is also essential to understand that taking psilocybin outside a controlled setting has risks, including experiencing various undesirable and harmful effects. Data available in scientific papers show encouraging therapeutic results. However, further and more robust trials are needed to better understand the therapeutic properties of psilocybin.
Acknowledgments: The authors acknowledge the technical support of “Association for the International Development of Academic and Scientific Collaboration – AIDASCO”.
References
- Gill, H.; Puramat, P.; Patel, P.; Gill, B.; Marks, C.A.; Rodrigues, N.B.; Castle, D.; Cha, D.S.; Mansur, R.B.; Rosenblat, J.D.; McIntyre, R.S. The Effects of Psilocybin in Adults with Major Depressive Disorder and the General Population: Findings from Neuroimaging Studies. Psychiatry Research 2022, 313, 114577.
- Madras, B. Psilocybin in Treatment-Resistant Depression. New England Journal of Medicine 2022, 378, 1708–1709.
- Zeiss, R.; Gahr, M.; Graf, H. Rediscovering Psilocybin as an Antidepressive Treatment Strategy. Pharmaceuticals 2021, 14, 985.
- Sharp, S.C.; Hellings, J.A. Efficacy and Safety of Selective Serotonin Reuptake Inhibitors in the Treatment of Depression in Children and Adolescents. Clinical Drug investigation 2006, 26, 247–255.
- Khawam, E.A.; Laurencic, G.; Malone, D.A. Side effects of antidepressants: an overview. Cleveland Clinic Journal of Medicine 2006, 73, 35161.
- Carhart-Harris, R.L.; Bolstridge, M.; Rucker, J.; Day, C.M.J.; Erritzoe, D.; Kaelen, M.; Bloomfield, M.; Rickard, J.A.; Forbes, B.; Feilding, A.; Taylor, D.; Pilling, S.; Curran, V.H.; Nutt, D.J. Psilocybin with psychological support for treatment-resistant depression: An open-label feasibility study. The Lancet Psychiatry 2016, 3, 619–627.
- Lowe, H.; Toyang, N.; Steele, B.; Valentine, H.; Grant, J.; Ali, A.; Ngwa, W.; Gordon, L. The Therapeutic Potential of Psilocybin. Molecules 2021, 26, 2948.
- Coppola, M.; Bevione, F.; Mondola, R. Psilocybin for Treating Psychiatric Disorders: A Psychonaut Legend or a Promising Thera-peutic Perspective. Journal of Xenobiotics 2022, 12, 41–52.
- Van Court, R.C.; Wiseman, M.S.; Meyer, K.W.; Ballhorn, D.J.; Amses, K.R.; Slot, J.C.; Dentinger, B.T.M.; Garibay-Orijel, R.; Uehling, J.K. Diversity, biology, and history of psilocybin-containing fungi: Suggestions for research and technological development. Fungal Biology 2022, 126, 308–319.
- Arce, J.M.R.; Winkelman, M.J. Psychedelics, Sociality, and Human Evolution. Frontiers in Psychology 2021, 12, 729425.
- Guzman, G. New Studies on Hallucinogenic Mushrooms: History, Diversity, and Applications in Psychiatry. International Journal of Medicinal Mushrooms 2015, 17, 1019–1029.
- Hofmann, A.; Frey, A.; Ott, H.; Petrzilka, T.; Troxler, F. Konstitutionsaufklärung und Synthese von Psilocybin. Experientia 1958, 14, 397–399.
- Tylš, F.; Páleníček, T.; Horáček, J. Psilocybin – Summary of knowledge and new perspectives. European Neuropsychopharmacology 2014, 24, 342–356.
- Gill, H.; Gill, B.; Chen-Li, D.; El-Halabi, S.; Rodrigues, N.B.; Cha, D.S.; Lipsitz, O.; Lee, Y.; Rosenblat, J.D.; Majeed, A.; Mansur, R.B.; Nasri, F.; Ho, R.; McIntyre, R.S. The emerging role of psilocybin and MDMA in the treatment of mental illness. Expert Review of Neurotherapeutics 2020, 20, 1263–1273.
- Shao, L.X.; Liao, C.; Gregg, I.; Davoudian, P.A.; Savalia, N.K.; Delagarza, K.; Kwan, A.C. Psilocybin induces rapid and persistent growth of dendritic spines in frontal cortex in vivo. Neuron 2021, 109, 2535–2544.
- Beïque, J.C.; Imad, M.; Mladenovic, L.; Gingrich, J.A.; Andrade, R. Mechanism of the 5-hydroxytryptamine 2A receptor-mediated fa-cilitation of synaptic activity in prefrontal cortex. Proceedings of the National Academy of Sciences 2007, 104, 9870–9875.
- Vollenweider, F.X., Kometer, M. The neurobiology of psychedelic drugs: Implications for the treatment of mood disorders. Nature Reviews Neuroscience 2010, 11, 642–651.
- Sakashita, Y.; Abe, K.; Katagiri, N.; Kambe, T.; Saitoh, T.; Utsunomiya, I.; Horiguchi, Y.; Taguchi, K. Effect of Psilocin on Extracellular Dopamine and Serotonin Levels in the Mesoaccumbens and Mesocortical Pathway in Awake Rats. Biological and Pharmaceutical Bulletin 2015, 38, 134–138.
- Gukasyan, N.; Davis, A.K.; Barrett, F.S.; Cosimano, M.P.; Sepeda,N.D.; Johnson, M.W.; Griffiths, R.R. Efficacy and safety of psilocybin-assisted treatment for major depressive disorder: Prospective 12-month follow-up. Journal of psychopharmacology 2022, 36, 151–158.
- Davis, A.K.; Barrett, F.S.; May, D.G.; Cosimano, M.P.; Sepeda, N.D.; Johnson, M.W.; Finan, P.H.; Griffiths, R.R. Effects of Psilocybin-Assisted Therapy on Major Depressive Disorder. JAMA Psychiatry 2021, 78, 481.
- Goodwin, G.M.; Aaronson, S.T.; Alvarez, O.; Arden, P.C.; Baker, A.; Bennett, J.C.; Bird, C.; Blom, R.E.; Brennan, C.; Brusch, D.; Burke, L.; Campbell-Coker, K.; Carhart-Harris, R.; Cattell, J.; Daniel, A.; DeBattista, C.; Dunlop, B.W.; Eisen, K.; Feifel, D.; Malievskaia, E. Single-Dose Psilocybin for a Treatment-Resistant Episode of Major Depression. New England Journal of Medicine 2022, 387, 1637–1648.
- Ross, S.; Bossis, A.; Guss, J.; Agin-Liebes, G.; Malone, T.; Cohen, B.; Mennenga, S.E.; Belser, A.; Kalliontzi, K.; Babb, J.; Su, Z.; Corby, P.; Schmidt, B.L. Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: A randomized controlled trial. Journal of Psychopharmacology 2016, 30, 1165–1180.
- Kraehenmann, R.; Preller, K.H.; Scheidegger, M.; Pokorny, T.; Bosch, O.G.; Seifritz, E.; Vollenweider, F.X. Psilocybin-induced de-crease in amygdala reactivity correlates with enhanced positive mood in healthy volunteers. Biological psychiatry 2015, 78, 572–581.
- Carhart-Harris, R.L.; Roseman, L.; Bolstridge, M.; Demetriou, L.; Pannekoek, J.N.; Wall, M.B.; Tanner, M.; Kaelen, M.; McGonigle, J.; Murphy, K.; Leech, R.; Curran, H.V.; Nutt, D.J. Psilocybin for treatment-resistant depression: fMRI-measured brain mechanisms. Scientific reports 2017, 7, 13187.
- Barrett, F.S.; Doss, M.K.; Sepeda, N.D.; Pekar, J.J.; Griffiths, R.R. Emotions and brain function are altered up to one month after a sin-gle high dose of psilocybin. Scientific Reports 2020, 10, 2214.
